When you’re living with multiple myeloma, you learn fast that bravery isn’t only for big moments. It shows up in the small choices, too, like filling a cup of water when you’re tired, or calling the clinic because “something feels off.”
With multiple myeloma kidney problems, those small choices matter. The kidneys don’t complain loudly at first. They whisper through signs of renal impairment like lab changes, darker urine, swelling, or a new wave of nausea. The good news is that many kidney setbacks can be prevented, or caught early, when you know what tends to tip the balance.
This is a guide for the real days, treatment days, and the days after, even in remission, when you’re trying to live your life while keeping one eye on your health.
How multiple myeloma threatens the kidneys (and why speed matters)
Your kidneys are like high-traffic filters. All day, they strain your blood, keep what you need, and send the waste out. Multiple myeloma, a cancer of plasma cells, can clog or irritate that filter from several directions at once. These cancerous plasma cells produce monoclonal proteins that overwhelm kidney function.
One major issue is extra proteins made by myeloma cells (often called free light chains). In high amounts, these proteins can overwhelm the kidney’s tiny tubes, specifically clogging the renal tubules in a condition known as cast nephropathy, like wet paper piling up in a drain. Add dehydration, infection, or high calcium, and the risk of acute kidney injury climbs.
This is why your care team often treats kidney strain as urgent. Current expert guidance emphasizes that the most direct kidney protection is fast, effective control of the myeloma, which often includes medications like bortezomib and dexamethasone to lower the level of free light chains, paired with supportive care like hydration and close monitoring. If you want the deeper medical framework behind that approach, the International Myeloma Working Group has a patient-facing summary on managing myeloma-related renal impairment.
Another hard truth, but also a hopeful one, is this: kidney function can improve when the myeloma comes under control. People can move from crisis labs to steadier numbers, step by step, week by week. That’s not just biology. That’s perseverance, backed by good medicine.
Hydration habits that support a stressed kidney

Hydration sounds almost too simple, until you’ve tried to do it while nauseated, busy, anxious, or worn out from treatment. Still, for many people with multiple myeloma, steady fluids are one of the most practical kidney-protection tools you have.
Many patients are encouraged to practice oral hydration (often around 2 to 3 liters a day), but the right amount depends on your body size, heart health, swelling, sodium levels, and what your labs are doing. Staying hydrated is particularly important if you experience hypercalcemia, which can further damage the kidneys. If your team has ever said “limit fluids,” follow that plan instead.
A few habits tend to work better than heroic efforts:
- Sip early, sip often. Large amounts at night can backfire if you’re up all night in the bathroom.
- Use urine color as feedback. Pale yellow usually means you’re on track. Dark yellow can be a dehydration warning.
- Pair fluids with routine. A glass with morning meds. Another with lunch. A refill when you check your next appointment.
- Plan for “fluid loss” days. Vomiting, diarrhea, fever, and sweats can dry you out quickly. Ask your clinic when you should switch to electrolyte drinks, or when you should call.
Hydration is also about courage, because it’s rarely dramatic. It’s the quiet choice to support your body when you’d rather tune out. If you’re struggling to keep fluids down, that’s not a character flaw. It’s a symptom, and you deserve help.
Medication pitfalls and the labs that catch trouble early
Common meds and procedures that can raise risk
Not every kidney problem is caused by myeloma alone. Sometimes the kidney is already strained, and a common medication pushes it over the edge. That’s why it’s smart to treat your med list like a living document.
Kidney health is monitored throughout the multiple myeloma journey, including during a bone marrow biopsy or preparation for a stem cell transplant.
Bring up kidney safety before you start, stop, or “just take” any of these:
NSAIDs: Drugs like ibuprofen and naproxen can reduce blood flow to the kidneys, especially when you’re dehydrated or on diuretics.
IV contrast dyes for CT scans or angiograms: Contrast is sometimes needed, and sometimes avoidable. Ask if your kidney numbers change the plan, and whether you need extra fluids before or after.
Certain antibiotics and antivirals: Some are harder on kidneys than others, especially in IV form. Your team can choose safer options when possible.
Diuretics (water pills): These can be appropriate, but they can also worsen dehydration if the dose is too strong for your current intake.
Bone-strengthening drugs like bisphosphonates: Some treatments for myeloma bone disease require kidney-based dosing. Tell your oncology team about any change in urine output or swelling.
Myeloma drugs like lenalidomide: These often require dose modifications if kidney function is low.
A solid review of how myeloma and kidney failure connect is available in this open-access medical review, which also discusses supportive steps like hydration and avoiding kidney-stressing drugs.
Kidney labs to watch (and how to read them without panic)
Labs are not grades. They’re signals. And with multiple myeloma kidney concerns, signals matter most when you watch trends over time. Keep an eye on related conditions like hypertension and anemia, which can further impact kidney health.
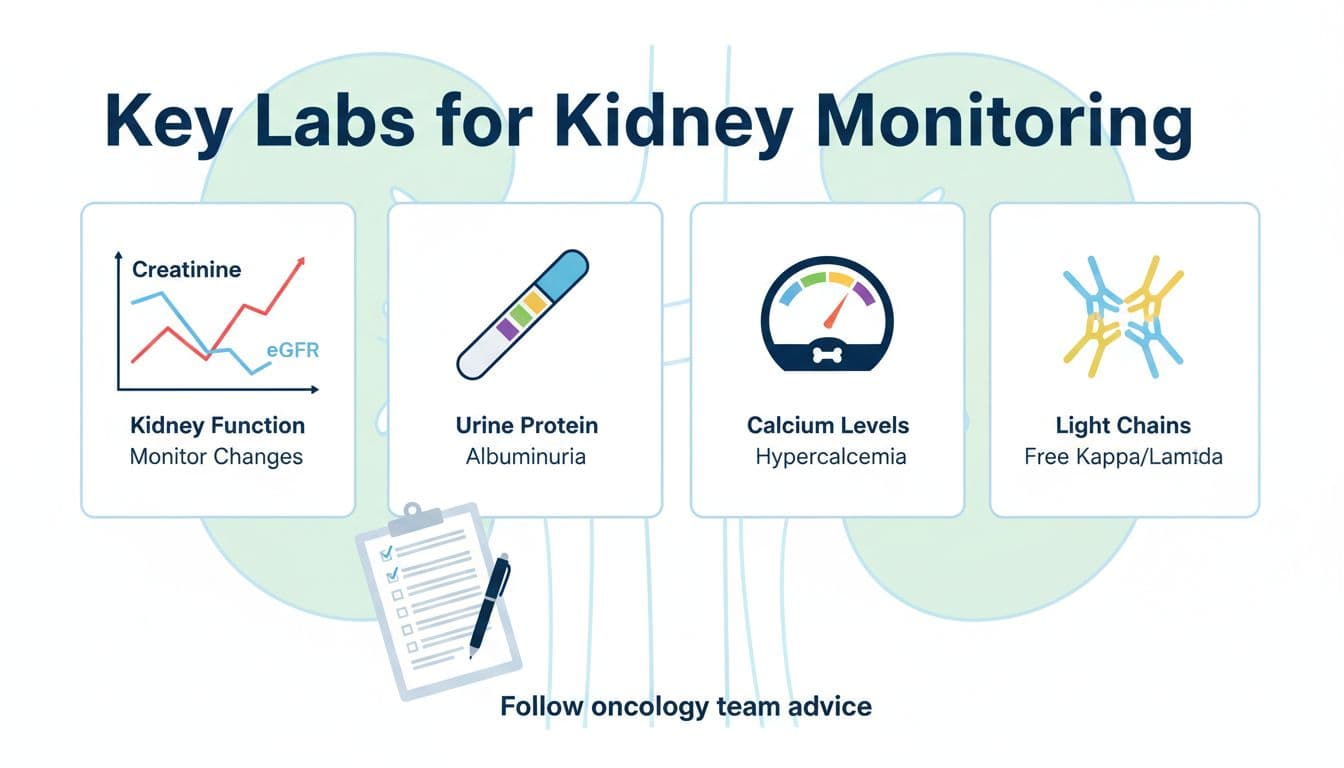
Here are the big ones many teams track:
| Lab or test | What it helps show | A question worth asking |
|---|---|---|
| Serum creatinine, eGFR, and creatinine clearance | Overall filtering function | “Is this change meaningful for me, or normal variation?” |
| BUN | Hydration status and waste buildup | “Could dehydration be part of this?” |
| Electrolytes (sodium, potassium, bicarbonate) | Salt and acid balance | “Do any meds need adjusting because of this?” |
| Calcium | High calcium can strain kidneys | “If calcium is high, what’s the plan today?” |
| Proteinuria (albumin or total protein) | Protein leaking into urine | “Do we need a proteinuria follow-up test?” |
| Serum free light chains | Multiple myeloma protein load that can harm kidneys | “How fast should we expect this to drop with treatment?” |
| Uric acid | Waste product buildup | “Is this high enough to need treatment?” |
| 24-hour urine (when ordered) | Total protein and myeloma proteins in urine | “What result would change my treatment plan?” |
For a patient-friendly walk-through, the International Myeloma Foundation explains blood tests used to assess kidney function. If you want a broader map of how myeloma testing fits together, the American Cancer Society’s overview of tests for multiple myeloma can help you make sense of the acronyms.
Call your team right away if you notice very low urine, new or fast swelling, confusion, severe nausea, or shortness of breath. Those can be signs the kidneys (or fluids) are in trouble, and waiting it out can cost time you don’t have. Severe cases may require dialysis or plasmapheresis.
Conclusion: Protecting your kidneys is a daily act of courage
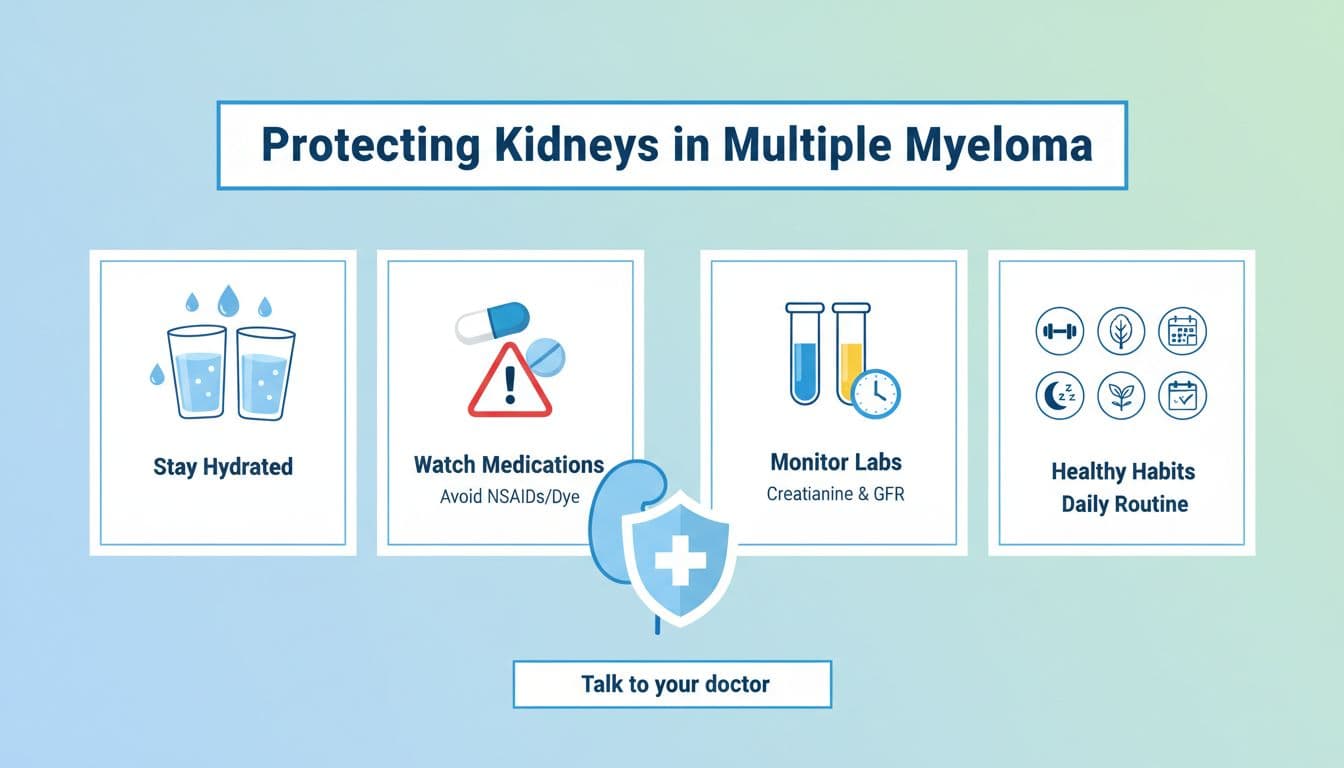
Kidney protection in multiple myeloma isn’t one perfect choice; it’s a string of steady ones: drink in a way your body can handle, treat “harmless” meds with respect, and keep an eye on the labs that tend to change first. If you’re in treatment or in remission, managing renal impairment remains a long-term part of your health journey, because the story can shift.
Most of all, remember this: you’re not overreacting when you ask questions or report symptoms. You’re practicing self-protection, and that is a form of courage that counts.

