There’s a special kind of bravery in waking up, planting your feet on the floor, and facing the day when your bones hurt. Multiple myeloma bone pain can feel personal, like your body is arguing with you about every step.
If you’re in treatment for Cancer, newly diagnosed, or living in remission, pain can mess with your sense of safety. It can also mess with your confidence. You start to wonder: Is this a normal ache, or a warning sign? Should I push through, or protect myself?
This guide is about the everyday kind of courage, the kind that looks like gentle movement, smart rest, and simple tracking so you can spot patterns and speak up early.
Why bone pain can flare during multiple myeloma treatment
Multiple myeloma often affects bones because myeloma cells can disrupt normal bone repair. That can lead to weak spots, tiny cracks, or fractures, most often in the spine, ribs, hips, and pelvis. Treatment can help control the disease, but pain doesn’t always leave on the same timeline.
Bone pain can also change because of:
- Healing and inflammation after procedures, injections, or radiation
- Muscle guarding, when your body tenses to protect a sore area
- Less activity, which can stiffen joints and tighten muscles
- Medication effects, like constipation or muscle aches that add “extra” discomfort
Pain is information, but it’s not always a clear message. That’s why you’ll do best with a plan you can repeat on hard days.
Safety first: signs that need urgent medical advice
Some pain is expected. Some pain is a red flag. Call your oncology team right away, or seek urgent care, if you notice:
- New weakness in an arm or leg
- Numbness or tingling that’s new or spreading
- Loss of bladder or bowel control
- Fever or chills along with pain
- Sudden severe pain, especially after a fall or twist
These can signal nerve pressure, infection, or a fracture. Getting checked quickly is a form of courage too.
Gentle movement for multiple myeloma bone pain (without “paying for it” later)

Movement can feel scary when bones are fragile. But total stillness often makes pain louder. Think of gentle motion like oil on a stiff hinge: not a fix, but a little ease.
A good goal is to move in ways that feel steady, not heroic.
Three simple ways to move on tender days
Short, flat walks: One to five minutes counts. Hallway laps count. Walking to the mailbox counts. If you use a cane or walker, that’s not “giving in”, it’s choosing stability.
Seated range-of-motion: Shoulder rolls, ankle pumps, slow knee lifts while seated. This helps circulation and reduces stiffness with less fall risk.
Light stretching: Gentle neck and chest opening, easy calf stretches, slow side bends only if approved. Skip deep twists or anything that “grabs” sharply.
For more patient-focused guidance on mobility and bone health, the Oncology Nursing Society has a helpful overview in their article on bone health, pain, and mobility recommendations for people with multiple myeloma.
The pacing rule that protects confidence
Try this simple check-in: stop while you still feel like you could do a little more. Pain often has a delay. Overdoing it can show up later like a storm rolling in after the sky looked clear.
If pain rises during movement, or your form changes (limping, hunching, holding your breath), that’s your cue to pause and reset.
Rest that protects bones (and still feels like living)
Rest is not quitting. Rest is how you give your bones a quieter environment to heal. The trick is to rest with support, not collapse into positions that strain your back or hips.
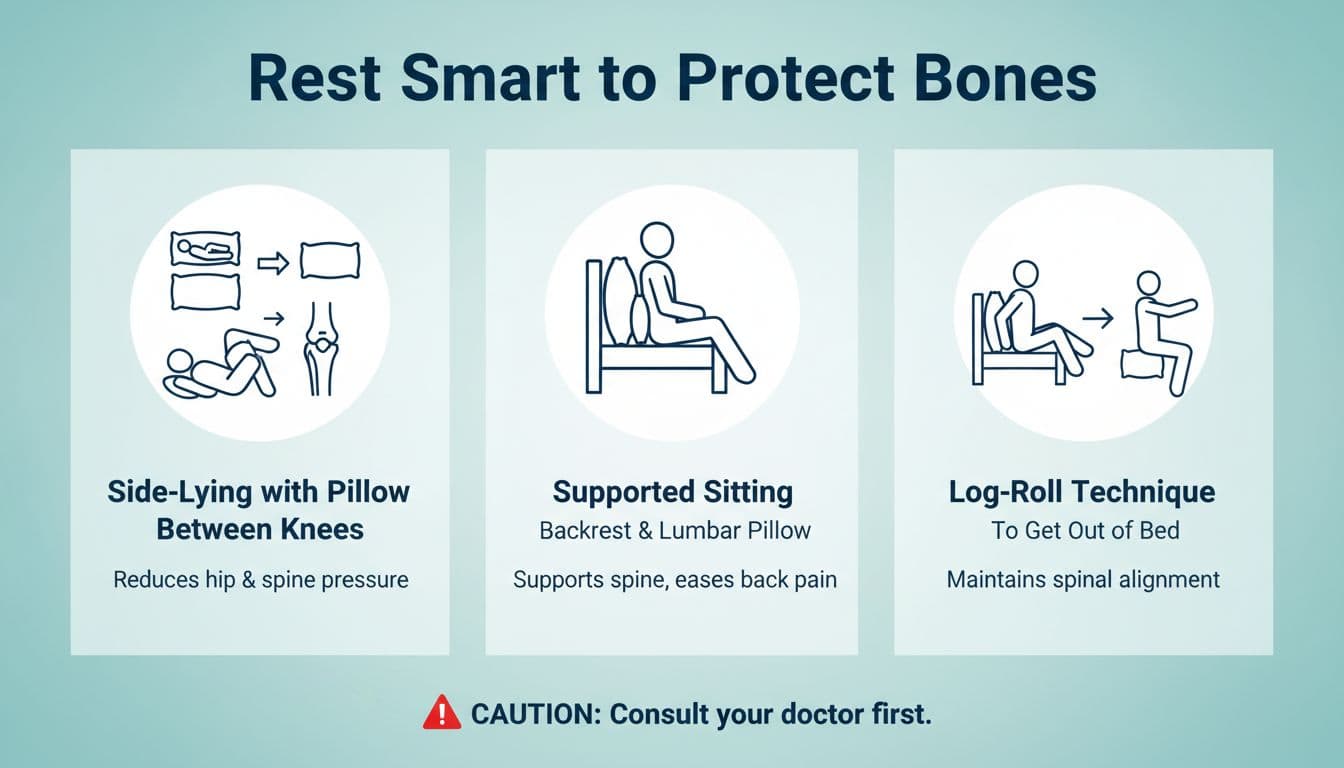
Positions many people find easier
Side-lying with a pillow between the knees: This can reduce pull on the low back and hips.
Supported sitting: A firm chair, feet flat, a small pillow or rolled towel behind the low back. Aim for relaxed shoulders and a neutral neck.
Log-roll to get out of bed: Roll onto your side first, then use your arms to push up as your legs swing down. It’s a small technique that can spare the spine.
Small comfort tools can help too: a heating pad on low (if approved), a cold pack for short bursts, and a “pillow map” that keeps you from waking up twisted.
If you’ve been told you have bone lesions or compression fractures, ask your team about bone-strengthening treatment and safety steps. The International Myeloma Foundation summarizes expert guidance in IMWG recommendations for treating myeloma-related bone disease.
Track triggers like a detective, not a judge
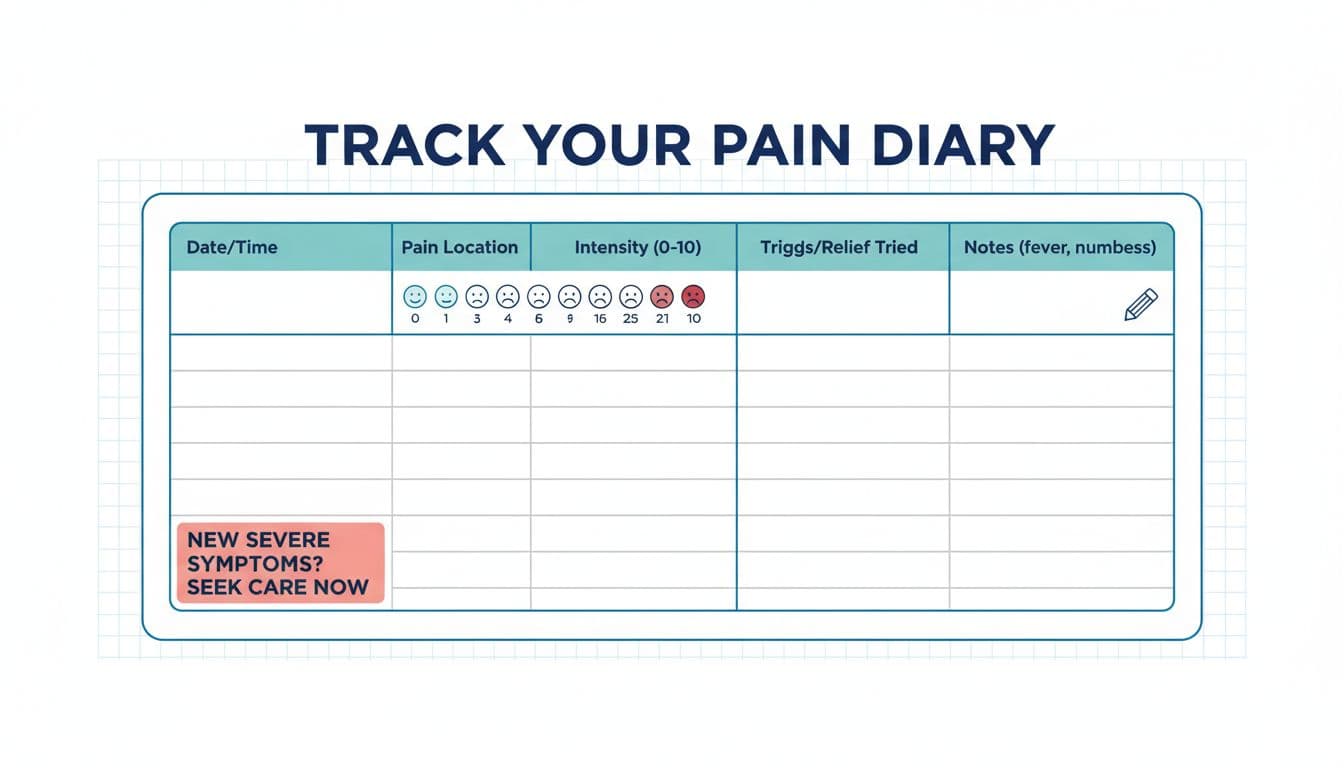
Pain can feel random until you write it down. Tracking isn’t about being perfect. It’s about giving your care team clean clues, especially when appointments are short and memories get fuzzy.
A simple pain diary can include:
| Date/time | Location | Intensity (0 to 10) | What you were doing | Meds or relief tried | Other symptoms |
|---|---|---|---|---|---|
A few patterns people often notice:
- Pain spikes after long sitting, then eases with short walks.
- Pain rises after new activity, especially bending or lifting.
- “Deep bone ache” days show up near treatment cycles or poor sleep.
- Constipation or dehydration makes everything feel worse.
Bring your notes to visits. It helps your team decide if you need imaging, a medication change, physical therapy, or added bone support. For a deeper medical review of approaches clinicians use, see the open-access article on pain management in multiple myeloma patients.
When to ask about medical pain control options
Your daily plan (move, rest, track) works best when pain is also treated medically. Depending on your situation, your team may discuss bone-protecting medicines (bisphosphonates or denosumab), pain relievers, radiation for a specific painful area, bracing, or other supports. Never start new over-the-counter meds without asking, because some options (like NSAIDs) can be risky for kidneys in certain patients.
If you want a plain-language overview of pain needs in myeloma care, this resource on management of pain in multiple myeloma can help you think through questions to bring to your next appointment.
Conclusion: courage is the plan you can repeat
Multiple myeloma bone pain can shrink your world, one careful movement at a time. Still, day by day, you can widen that world again with gentle motion, supported rest, and simple tracking that turns confusion into usable facts.
If you’re in treatment or in remission, keep choosing the steady next step. Keep telling your team what’s changing. Courage isn’t pretending it doesn’t hurt, it’s learning what helps, and doing it again tomorrow.

