A Cancer diagnosis asks you to be brave in ways you never trained for. Not the movie kind of brave, with big speeches and bright lights, but the quiet kind. The kind that shows up when you swallow a new pill, sit through an infusion, or notice a new ache and decide not to ignore it.
One of the most important “don’t-ignore-it” topics during treatment is blood clots. Many people hear the words and picture something rare. It isn’t. Blood clots can happen during treatment, after surgery, and sometimes even when you’re feeling better or in remission.
This guide covers what blood clots are, why risk is higher, the warning signs to watch for, how prevention really works, and how to travel more safely when Cancer is part of your life.
Why blood clot risk is higher during Cancer treatment
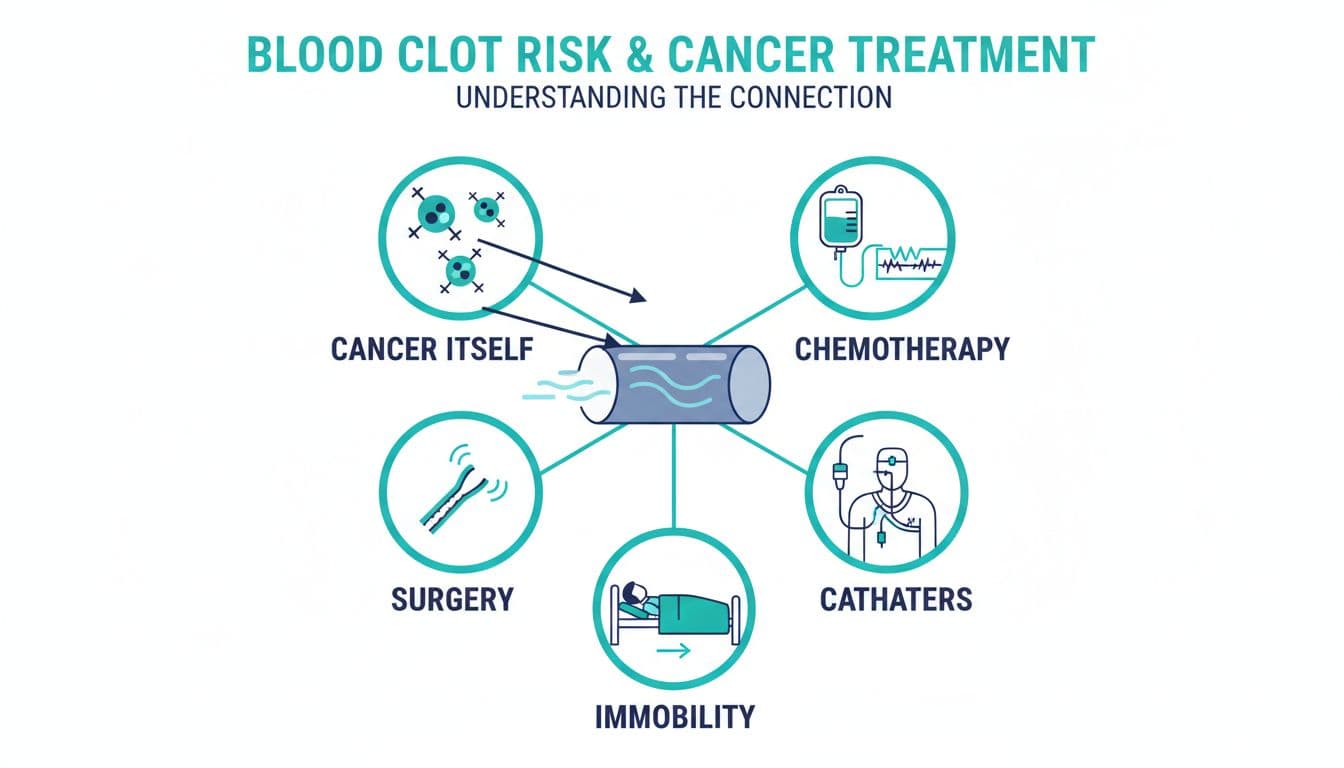
Think of your bloodstream like a river. Most days it flows smoothly. Cancer can make that flow “stickier,” and some treatments can rough up the riverbanks (your blood vessels). Add time spent resting or recovering, and the current can slow.
That’s why blood clots cancer risk is a real part of care, not a side note. Recent reporting continues to describe clots (often called VTE, which includes DVT and PE) as a major cause of serious illness in people with Cancer. One current estimate notes about 3% of patients develop a clot in the year after diagnosis, and risk is far higher than in people without Cancer.
Common reasons risk rises include:
- Cancer itself, which can change how blood clots.
- Chemotherapy and other drugs, which can irritate vessels and shift clotting balance.
- Surgery, especially abdominal or pelvic procedures, plus recovery time.
- Central lines, ports, or catheters, which can irritate veins.
- Less movement, from fatigue, hospital stays, long car rides, or flights.
For a clear overview of risk factors and how clinicians think about clot risk in Cancer, the CDC’s guidance on blood clots with cancer is a reliable place to start.
The two clots you hear about most: DVT and PE
A clot can form in a deep vein, often in the leg. That’s deep vein thrombosis (DVT). The danger is that part of that clot can break off, travel to the lungs, and block blood flow. That’s pulmonary embolism (PE).
DVT is the spark, PE is the fire.
People sometimes assume they’ll “just know” if a clot is happening. Sometimes you will. Sometimes symptoms are quiet, or they look like normal treatment side effects. That’s why patterns matter, especially new, one-sided, or sudden changes.
Warning signs of blood clots (what to watch for today)
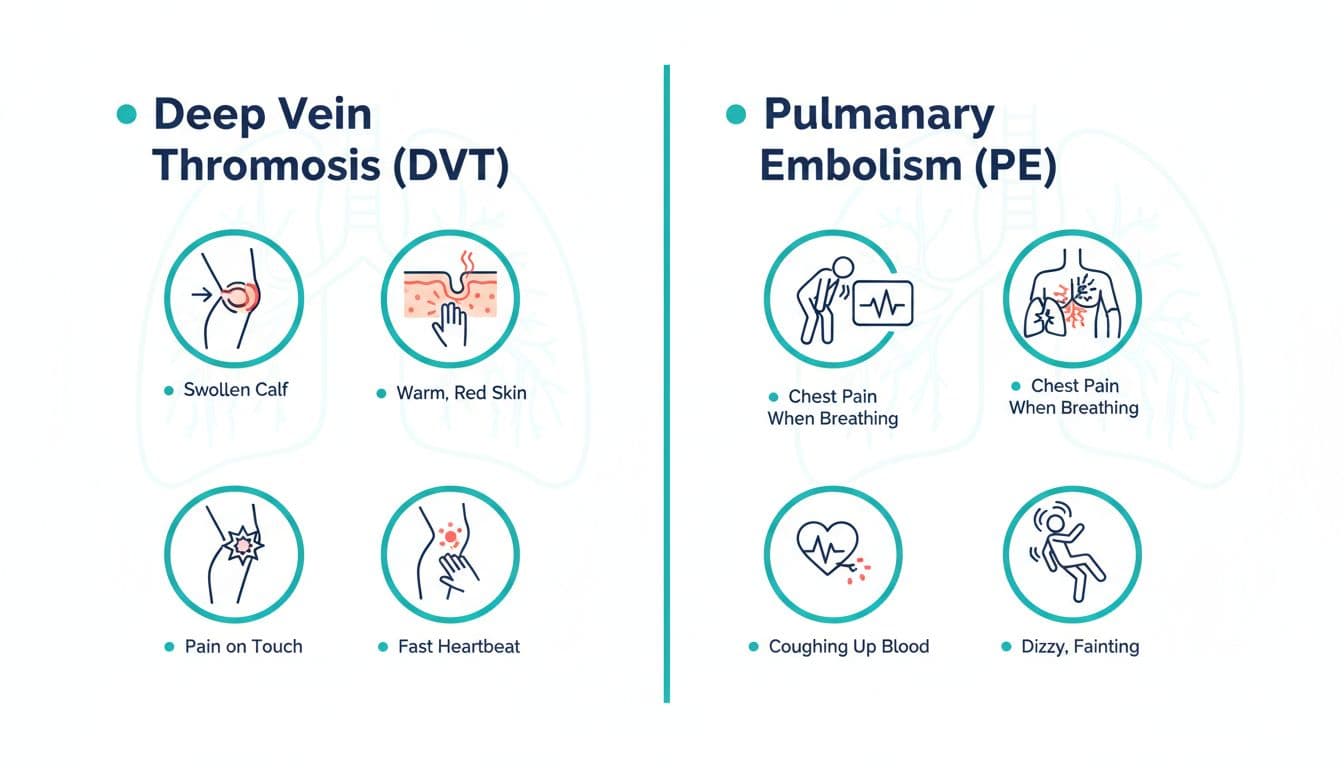
Here’s a simple way to hold it in your mind: leg clues and lung clues.
DVT warning signs (usually in one leg)
- Swelling in the calf, ankle, or thigh (often one-sided)
- Warmth or redness over a vein
- Pain, cramping, or tenderness that wasn’t there before
- A “heavy” feeling in one leg
PE warning signs (lungs and heart strain)
- Sudden shortness of breath, even at rest
- Chest pain that’s worse when you breathe in
- Fast heartbeat, new dizziness, or fainting
- Coughing up blood
If you have PE symptoms, treat it as an emergency and call local emergency services right away. This is one of those moments where courage is simple: you act, even if you’re not sure.
If you’re unsure how your symptoms fit into the bigger picture, Cancer Research UK’s overview of cancer and blood clot risk explains DVT and PE in plain language.
Prevention that fits real life (not perfection)
Prevention isn’t about doing everything. It’s about doing the right things for your body, your treatment plan, and your bleeding risk.
Medication prevention (anticoagulants)
Some people need blood thinners during treatment or after surgery. If your team prescribes them, take them exactly as directed and don’t change the dose on your own. Blood thinners can lower clot risk, but they also raise bleeding risk, so your care team is always balancing both.
Newer research has also focused on how long people should stay on treatment if they’ve already had a clot, including whether a reduced dose after the first months may keep protection while lowering bleeding risk for some patients. Your case is personal, so let your oncology or hematology team guide the plan.
For practical patient-focused guidance on anticoagulants and clot care during treatment, MD Anderson’s page on blood clots and anticoagulants is a helpful reference.
Movement prevention (small counts)
You don’t need a workout. You need circulation.
Try this rule of thumb: if you’ve been still for an hour, move for a couple minutes. Walk to the mailbox, do a lap around the kitchen, flex your ankles in bed. These are tiny acts, but they add up.
Hydration and comfort
Dehydration can thicken blood, and treatment can make hydration hard. Sipping regularly can be more realistic than forcing big glasses.
Also pay attention to clothing. Tight waistbands or socks that pinch can make swelling worse, especially after surgery or with lymph node removal.
Compression socks (only with approval)
Compression socks can help some people, but they aren’t for everyone. If you might already have a clot, compression can be unsafe. Ask your clinician first, especially if you have leg swelling, neuropathy, or circulation problems.
Travel tips during treatment and in remission (planes, cars, and “I just need a break”)
Travel can feel like a small return to yourself. It can also come with long stretches of sitting, which increases clot risk for anyone, and more so during Cancer care.
The goal isn’t to cancel your life. The goal is to travel with a plan.
Before you book
- Ask your care team if travel is safe right now, especially after surgery, with low platelets, or while starting a new drug.
- If you’ve had a clot before, ask what to do if symptoms return while away.
- Pack meds in your carry-on, with extra doses in case of delays.
During the trip
On flights or long car rides, movement is your best tool.
- Choose an aisle seat if you can.
- Stand up and walk about every 1 to 2 hours when safe.
- Do ankle circles and heel raises in your seat.
- Drink water regularly, go easy on alcohol.
For detailed, practical guidance written for patients, the American Society of Hematology page on blood clots and travel lays out what helps and what doesn’t.
Know your “what if”
Save your oncology clinic number and know the emergency number for the country you’re visiting. If you’re traveling alone, tell one person your plan, where your meds are, and what symptoms would mean “we go now.”
That’s not anxiety. That’s preparation.
If you’re in remission: why clot awareness still matters
Remission can feel like exhaling after holding your breath underwater. But your body may still be recovering, and some risks don’t vanish on the day you ring a bell.
If you have a history of clots, a central line, hormone therapy, recent surgery, or ongoing fatigue that limits movement, keep clot signs on your radar. Mention any new leg swelling or unexplained shortness of breath quickly, even if you worry you’ll sound dramatic.
Courage, here, is letting your “new normal” include paying attention.
Conclusion
Blood clots during Cancer treatment are scary, but they’re also often preventable and treatable when caught early. Learn the warning signs, keep movement and hydration simple, follow your plan for anticoagulants, and travel with a few smart guardrails. If you’re in treatment or in remission, your body deserves that kind of steady care. The bravest question to ask yourself is sometimes the plainest one: “Is this new, and do I need help right now?”

