Waiting for a scan can feel like standing at the edge of a dark room, hand on the light switch, bracing for what you might see. In Cancer care, imaging isn’t just “pictures.” It’s a way your team asks the body careful questions, then listens for honest answers.
And courage shows up here in ordinary ways. It’s showing up hungry for a morning PET scan. It’s lying still when your mind wants to run. It’s walking back into a scanner even after you’ve heard hard news before, or even when you’re in remission and thought you might be done with all this.
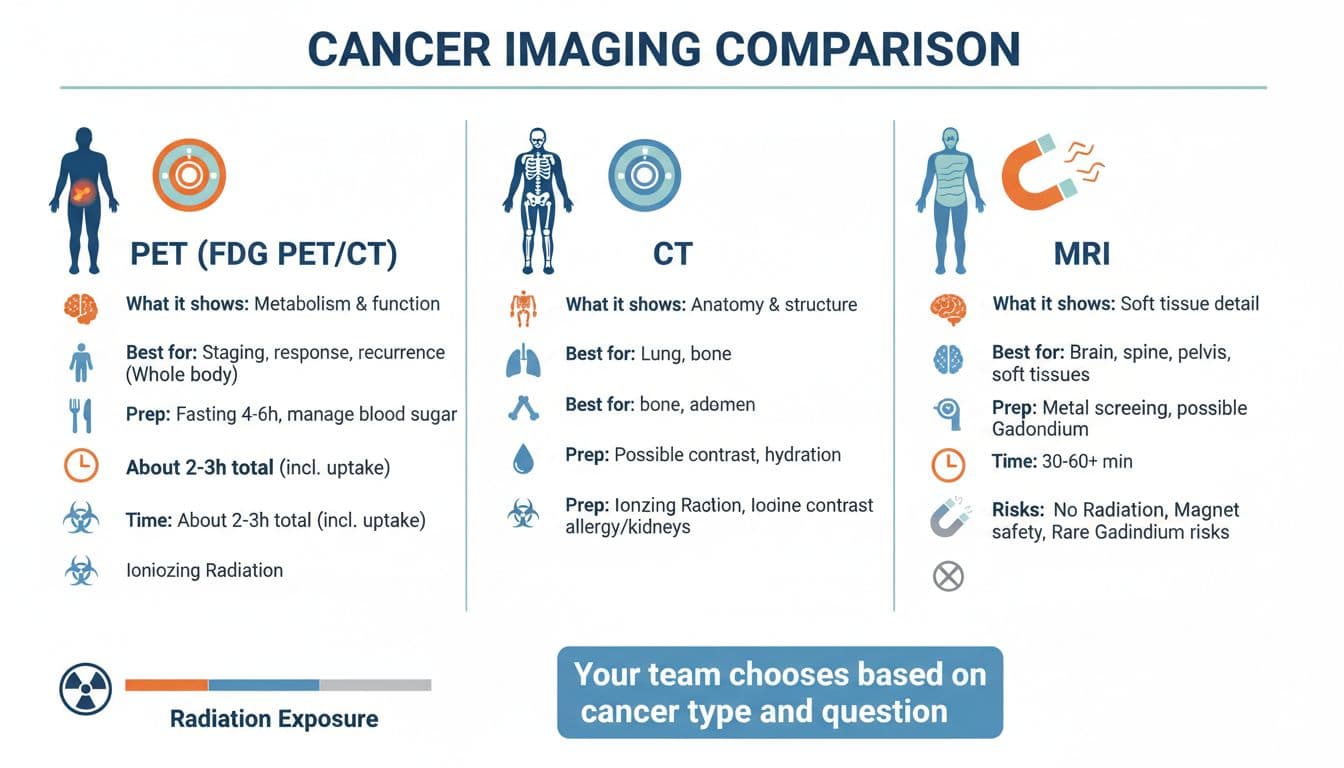
This guide breaks down PET, CT, and MRI, what each one checks, why your doctor might choose it, and how to prep without feeling like you need a medical dictionary.
Why your care team uses different scans (and why that’s not “mixed messages”)
Think of imaging like three different kinds of maps:
- CT is a fast road map of body structures.
- MRI is a detailed close-up map of soft tissues.
- PET (often PET/CT) is a “heat map” showing how active certain cells are.
Most of the time, your doctor isn’t ordering more tests because they’re unsure. They’re being precise. One scan may be best for spotting a mass, another for measuring it, and another for checking if treatment is working.
For a clear overview of how doctors choose between CT and MRI, Memorial Sloan Kettering’s explainer is helpful: CT scan vs. MRI differences and how doctors choose.
CT scan during cancer care: what it checks, when it helps most
A CT scan (computed tomography) uses X-rays to create detailed cross-section images. It’s often the workhorse for staging, checking for spread, and watching how tumors change over time.
What CT checks well
- Size and shape of tumors (anatomy)
- Lungs, liver, lymph nodes, and many abdominal areas
- Bone changes in some cases (though other tests may be better for certain bone questions)
What it’s like You lie on a table that moves through a donut-shaped scanner. Most CT scans are quick, often finished in minutes.
Contrast (the “dye”) Some CT scans use iodine-based contrast through an IV, or oral contrast for the belly. Contrast can make certain tissues stand out.
Tell your team if you:
- Have had a contrast reaction before
- Have kidney disease
- Take diabetes meds like metformin (your team will tell you if any pause is needed)
MRI during cancer care: when detail matters most
An MRI (magnetic resonance imaging) uses a strong magnet and radio waves, not radiation. MRI shines when your doctors need a sharper view of soft tissue.
What MRI checks well
- Brain and spinal cord
- Pelvis (prostate, cervix, uterus, rectum)
- Breast tissue, liver lesions, and many soft-tissue questions
- Nerves, muscles, and joints near a tumor
What it’s like MRI usually takes longer than CT. The scanner is a tube, and it can be loud. You’ll need to lie still. If you’re prone to claustrophobia, say so early. Many centers can offer music, mirrors, or medicine to help you stay calm.
MRI contrast (gadolinium) Some MRIs use gadolinium contrast. It’s not the same as CT contrast. Your team may check kidney function first, especially if you have kidney problems.
For a patient-friendly comparison of how MRI, CT, and PET are used, this overview from UNC Health Appalachian can add context: comparing MRI, CT, and PET scans and when they’re used.
PET scan (often PET/CT): what it checks that CT and MRI can’t
A PET scan (positron emission tomography) looks at function, not just form. Most cancer PET scans use a sugar-like tracer called FDG. Cells that use a lot of sugar may “light up,” which can help your doctors spot active disease.
PET is often paired with CT as PET/CT, combining activity (PET) with location (CT).
What PET checks well
- Whether a spot is metabolically active (more like “is it busy?” than “what does it look like?”)
- Possible spread to lymph nodes or distant sites (staging)
- Treatment response, especially when tumor size changes slowly
- Possible recurrence when symptoms or labs raise concerns
What it’s like PET/CT is usually a longer appointment. After the injection, you rest quietly while the tracer circulates (often around an hour). Then you’ll be scanned.
If you want a deeper patient overview of PET/CT in cancer, including how it compares with CT and MRI, this is a solid read: PET/CT scan for cancer (PET vs CT vs MRI).
PET vs CT MRI at a glance (what each one answers)
| Scan | Best at showing | Common uses in cancer care | Radiation? | Typical time |
|---|---|---|---|---|
| CT | Anatomy, size, location | Staging, follow-up, lung and abdomen checks | Yes | Often 10 to 30 minutes |
| MRI | Soft-tissue detail | Brain, spine, pelvis, certain liver or breast questions | No | Often 30 to 60+ minutes |
| PET/CT | Activity plus anatomy | Staging, response, suspected recurrence | Yes (usually more than CT alone) | Often 2 to 3 hours total |
Your team’s choice is often about one thing: What question are we trying to answer today?
How to prep for PET, CT, and MRI (simple steps that make scans clearer)
Prep can feel like another test you might fail. You won’t. You’re just helping the scanner do its job.
PET/CT prep (common FDG PET rules)
Most centers ask you to:
- Fast 4 to 6 hours before (water is usually OK). Avoid candy, gum, coffee with sugar, and anything with calories.
- Skip hard workouts for about 24 hours before, since muscles can take up tracer.
- Avoid high-sugar and high-carb foods the day before if your team advises it.
- Dress warm and stay comfortable, since being cold can affect tracer uptake in brown fat.
- If you have diabetes, your instructions may be different. Many places adjust timing for insulin or pills to help keep blood sugar in range. Follow your imaging team’s plan, not generic rules.
Plan for a longer visit: check-in, IV, resting time after injection, then the scan.
CT prep (with or without contrast)
CT prep depends on the body part and whether contrast is used.
- You may be asked to hydrate well, especially if IV contrast is planned.
- Some CT exams require fasting for a few hours, others don’t.
- Tell your team about kidney disease, past contrast reactions, and all meds.
Many people feel a brief warm flush with IV contrast. That can be normal, but speak up if you feel itchy, tight in the throat, or short of breath.
MRI prep (metal matters)
MRI is mostly about safety.
- Remove all metal (jewelry, hairpins, watches, some clothing with metal parts).
- Tell the team about implants (pacemakers, cochlear implants, aneurysm clips), shrapnel, or metal work exposure.
- If contrast is planned, you may have a kidney blood test first.
- If you’re anxious in tight spaces, ask ahead about options (open MRI, music, a support person, or medicine).
The quiet kind of courage: getting through scan day
Scan days can bring “scanxiety,” even if you’ve done this before. Even if you’re in remission. Even if your last results were good. The mind remembers.
A few grounded strategies can help:
- Bring a small comfort routine, a playlist, a soft sweater, a scent-free lotion for after.
- Ask the tech what to expect next, step by step. Knowing the order can calm the body.
- If waiting for results is the hardest part, ask your clinic how and when results are released, and who will call.
Courage doesn’t always roar. Sometimes it’s just you showing up anyway.
Conclusion
PET vs CT MRI isn’t a contest, it’s a set of tools, each with a different kind of truth to offer. CT measures structure, MRI reveals fine detail, and PET helps show activity that can guide big decisions. If you prep the way your team asks, you’re doing your part, even when it’s tiring. Keep asking questions until you feel steady, because clarity is a form of care too.

