You open the portal, and there they are, rows of numbers that look like a math test you didn’t study for. It’s a strange moment, quiet and loud at the same time.
During Cancer treatment, lab work can feel like a weekly verdict. But most of the time, your CBC and CMP aren’t judging you. They’re checking on you, like a nurse popping in to ask, “How’s your body holding up today?”
This guide breaks down common CBC CMP results in plain language, with the one idea many people need most: the goal isn’t perfect numbers, it’s safe treatment, steady recovery, and a path forward, including when you’re in remission and still being watched closely.
CBC and CMP during cancer treatment: why so many blood draws?
Treatment asks a lot of your body. Chemo can slow down bone marrow. Some meds stress the liver. Diarrhea and vomiting can shift salts and fluids. Even not eating well for a week can show up on paper.
That’s why your team orders labs so often. These tests help them decide things like:
- Is it safe to give the next dose today?
- Do we need fluids, a transfusion, or a medication change?
- Is a fever more risky because your infection-fighting cells are low?
If you want a reliable overview of how labs are used in care, the American Cancer Society’s guide to understanding lab test results is a helpful, steady resource.
CBC vs CMP, a quick map of what each test checks
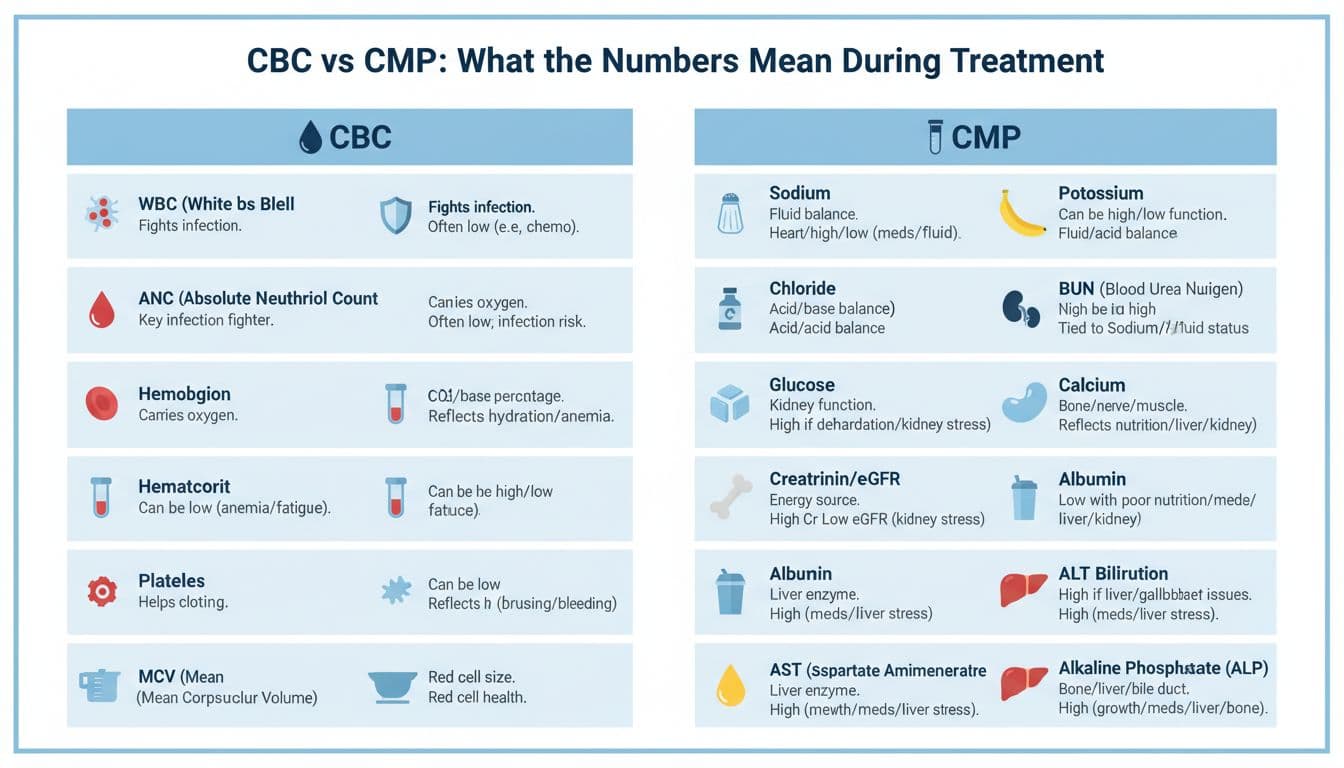
Think of the CBC and CMP like two quick “status reports” from different parts of your body.
| Test | What it mostly watches | What it often helps with during treatment |
|---|---|---|
| CBC (Complete Blood Count) | Bone marrow output (blood cells) | Infection risk, anemia, bleeding risk |
| CMP (Comprehensive Metabolic Panel) | Chemistry (kidneys, liver, salts, sugar, proteins) | Hydration status, organ stress, medication safety |
| Both together | A wider safety picture | Timing, dosing, and supportive care decisions |
The CBC is about your blood cells. The CMP is about the chemistry that keeps those cells (and everything else) working.
CBC numbers made simple (the ones people worry about most)
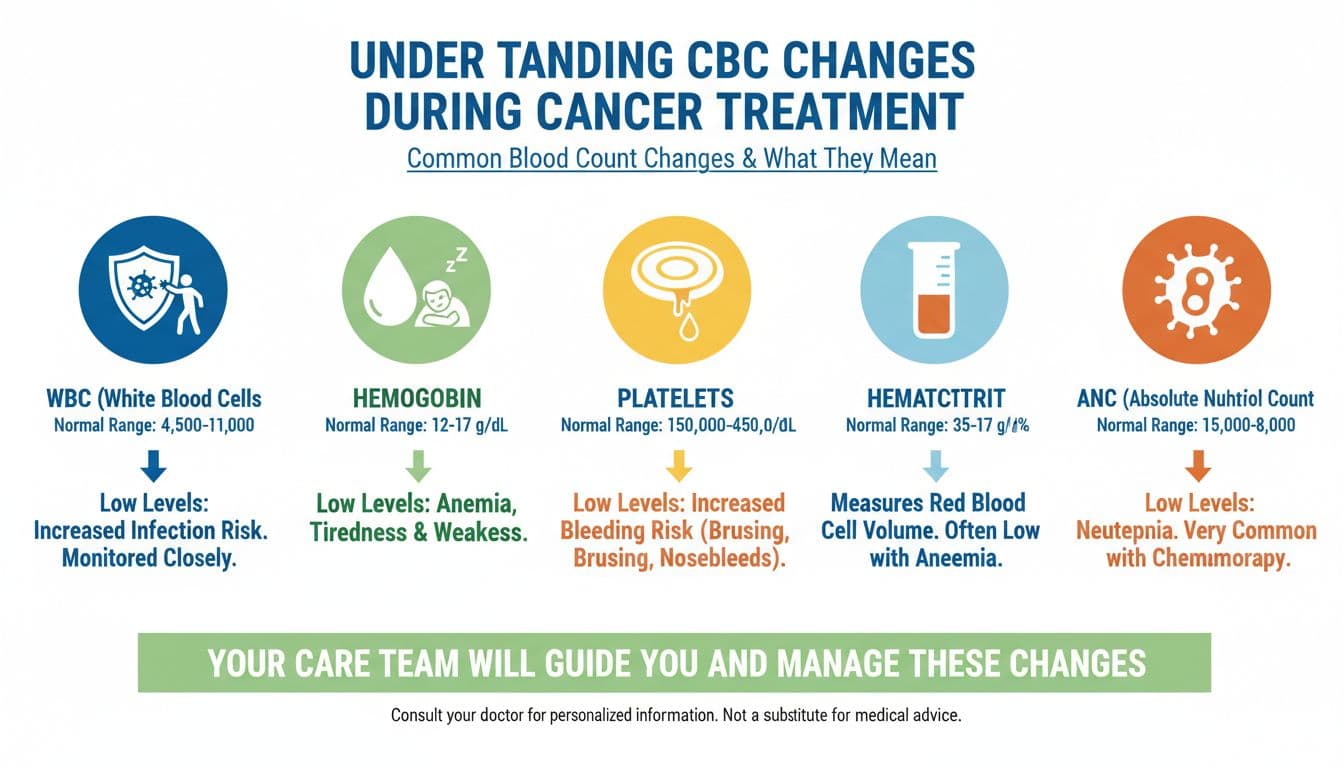
A CBC usually includes white blood cells, red blood cells, and platelets. During treatment, it’s normal to see movement. Courage sometimes looks like watching those swings and still showing up.
For a clear definition of what a CBC measures, the Canadian Cancer Society’s CBC page is straightforward and patient-focused.
WBC and ANC: “How ready am I to fight infection?”
- WBC (white blood cell count) is the big bucket number.
- ANC (absolute neutrophil count) is often the one your team tracks most closely, because neutrophils are front-line infection fighters.
When ANC is low, your care team might delay treatment, lower a dose, or give a growth-factor shot. This is not a setback in character. It’s a safety call.
If you’ve been told you’re “neutropenic,” that word can land hard. Still, the practical meaning is simple: your body has fewer guards on duty right now.
Hemoglobin and hematocrit: “Why am I so tired?”
- Hemoglobin carries oxygen.
- Hematocrit is related, it reflects how much of your blood is made up of red blood cells.
When these drop, people often feel wiped out, short of breath, or lightheaded. Low numbers can come from treatment effects, bleeding, or the cancer itself, and your team looks at the whole story before acting.
Sometimes courage is not pushing through. It’s telling the truth about fatigue, and letting your team help.
Platelets: “Am I more likely to bruise or bleed?”
Platelets help your blood clot. When platelets are low, you might notice bruising, nosebleeds, bleeding gums, or tiny red-purple spots on the skin.
Low platelets can lead your team to pause treatment or recommend a transfusion. You may also be asked to avoid certain meds that raise bleeding risk.
MCV (and other red cell details): “What kind of anemia is this?”
MCV describes the average size of your red blood cells. It doesn’t usually drive same-day decisions by itself, but it can hint at patterns, like anemia related to treatment, nutrition, or long-term inflammation.
If your MCV is flagged, it’s often a clue for a slower conversation, not a fast emergency.
CMP numbers made simple (kidneys, liver, salts, and fuel)
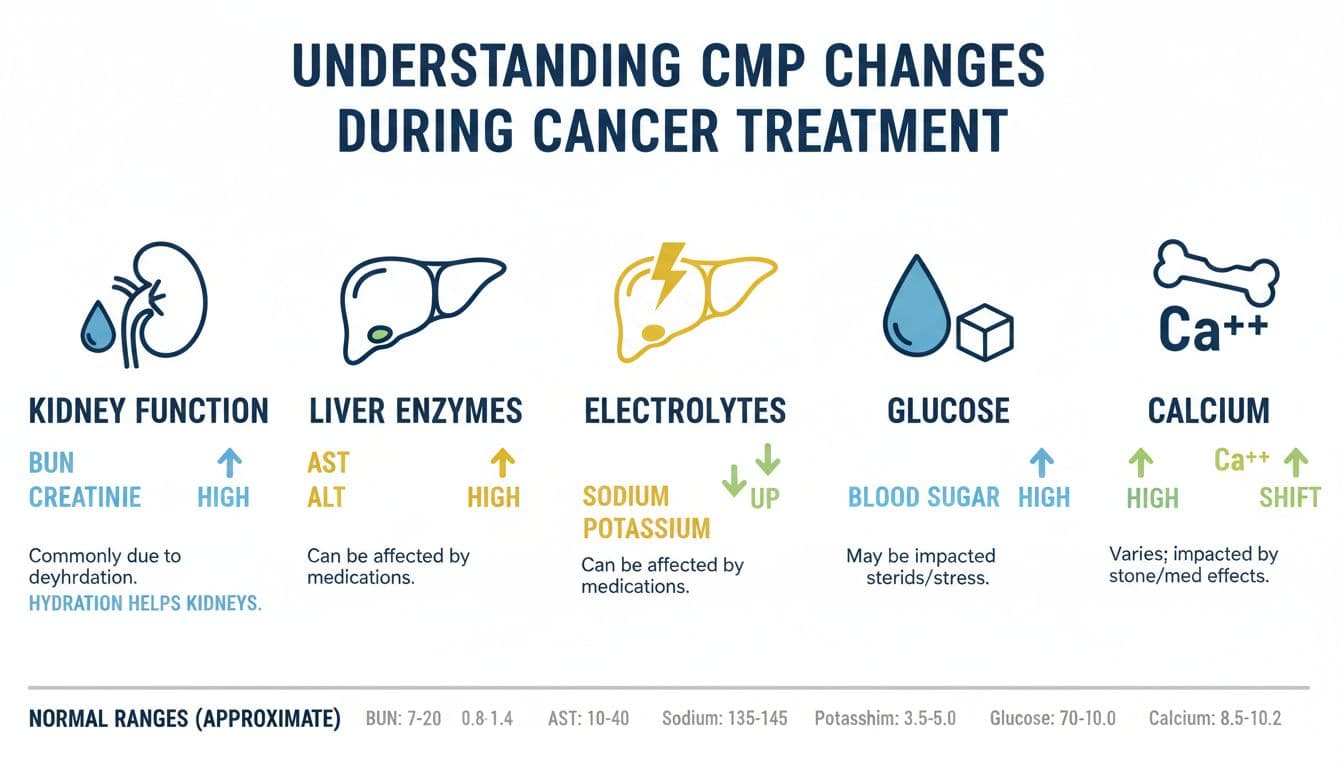
The CMP can look like a long list, but it’s really a few themes repeated in different ways. For a dependable, plain-language overview, MedlinePlus has a solid page on the Comprehensive Metabolic Panel (CMP).
Electrolytes (sodium, potassium, chloride, CO2): “Are my fluids and salts balanced?”
Electrolytes help with nerve signals, muscle function, heart rhythm, and fluid balance.
During treatment, electrolytes can shift because of dehydration, vomiting, diarrhea, poor intake, or certain meds. When something is off, the fix might be as simple as fluids, food changes, or supplements, but your team decides based on your whole picture.
Kidney markers (BUN, creatinine, sometimes eGFR): “Are my kidneys keeping up?”
- Creatinine rises when kidneys aren’t filtering as well.
- BUN can rise with dehydration, among other causes.
One common, very human reason for abnormal kidney numbers during treatment is not drinking enough because everything tastes wrong, nausea is constant, or you’re just tired of forcing water.
Kidney numbers can also guide drug dosing, since some meds clear through the kidneys.
Liver tests (AST, ALT, alkaline phosphatase, bilirubin): “Is my liver irritated or blocked?”
The liver handles many medications. Temporary enzyme bumps can happen with treatment, infections, or other meds you’re taking.
- AST and ALT often rise with liver irritation.
- Bilirubin is tied to bile flow and red blood cell breakdown.
- Alkaline phosphatase can rise for several reasons, including liver and bone sources.
A single abnormal result doesn’t automatically mean damage. Your team often looks for trends, symptoms, and how high the value is.
Proteins (albumin, total protein): “Do I have enough building blocks?”
Albumin is influenced by nutrition, inflammation, and fluid status. When it’s low, people sometimes notice swelling, or they simply feel weaker and slower to bounce back.
Low albumin can be a nudge toward extra nutrition support, not a sign you’ve failed at eating. Treatment can make food feel like a chore.
Glucose and calcium: “Is my body getting steady fuel?”
- Glucose can run high with steroids or stress, and low if you aren’t eating.
- Calcium can shift with hydration changes and other conditions your team considers.
These are usually managed in context, not in isolation.
Trends matter more than one result
It’s easy to stare at a red flag and panic. But your clinicians often care more about:
Direction: Are values dropping fast, rising slowly, or stable?
Timing: Does this line up with your chemo cycle (like a “nadir” week)?
Symptoms: Fever, bleeding, chest pain, confusion, new shortness of breath.
Risk: What’s safe for treatment today?
If you’re in remission, labs can still bounce around, especially if you’re rebuilding strength, changing meds, or recovering from months of strain. Ongoing monitoring isn’t a sign of doom. It’s the follow-through that keeps you safe.
Questions to bring to your next appointment (so the numbers feel less powerful)
When you’re staring at your CBC CMP results, it helps to have a script. Consider asking:
“Which number matters most for my next step?”
“Is this change expected for my treatment week?”
“What symptoms would make this urgent?”
“Are we watching a trend or reacting to a one-time blip?”
“What can I do this week that actually helps (fluids, food, rest, meds)?”
Write the answers down. Stress steals memory, and you shouldn’t have to hold it all in your head.
Conclusion
Lab results can feel like a spotlight, harsh and unforgiving. But most of the time, they’re more like a dashboard, showing what your body needs so your team can adjust the plan. With time, patterns start to make sense, and the fear loosens its grip.
Keep asking for clarity, keep tracking trends, and keep honoring the quiet courage it takes to face the numbers, whether you’re mid-treatment or in remission and still showing up for follow-ups.

