When you’re living with multiple myeloma therapy decisions, time starts to feel different. Some days move like thick syrup. Other days pass in a blur of lab results, pill bottles, and waiting rooms. And in the middle of it all, there’s a quiet question that keeps returning: what does courage look like now?
Not the movie version. The everyday version. The courage it takes to answer the phone, to show up for another blood draw, to keep eating when nothing tastes right, to keep hoping when your mind wants to sprint to worst-case thoughts.
If you’ve heard someone mention “Byte Therapy” for multiple myeloma, you’re not alone. The name sounds like computers, but most of the time people mean BiTE therapy, a newer immune treatment that helps your body’s T cells recognize and attack myeloma cells. Let’s talk about what that means, in plain language, and how people are using real “bytes” (simple tech tools) to make treatment feel more manageable.
Multiple myeloma: a Cancer that asks a lot of the body (and the spirit)
Multiple myeloma is a blood Cancer that starts in plasma cells, a kind of white blood cell in the bone marrow. When myeloma cells build up, they can crowd out healthy blood-making cells and affect bones, kidneys, and immune function. That’s the medical side.
The human side is harder to chart. Pain that changes your posture. Fatigue that doesn’t care about your plans. The emotional whiplash of hearing “stable” one month and “progression” the next.
Courage, here, is often private. It can look like letting someone else drive. It can look like asking the nurse to repeat something. It can look like saying, “I’m scared,” without trying to clean it up.
What people mean by “Byte Therapy”: BiTE therapy in plain words
“Byte Therapy” isn’t a standard medical term. In myeloma clinics, the treatment people are usually referring to is BiTE therapy, short for bispecific T-cell engager therapy.
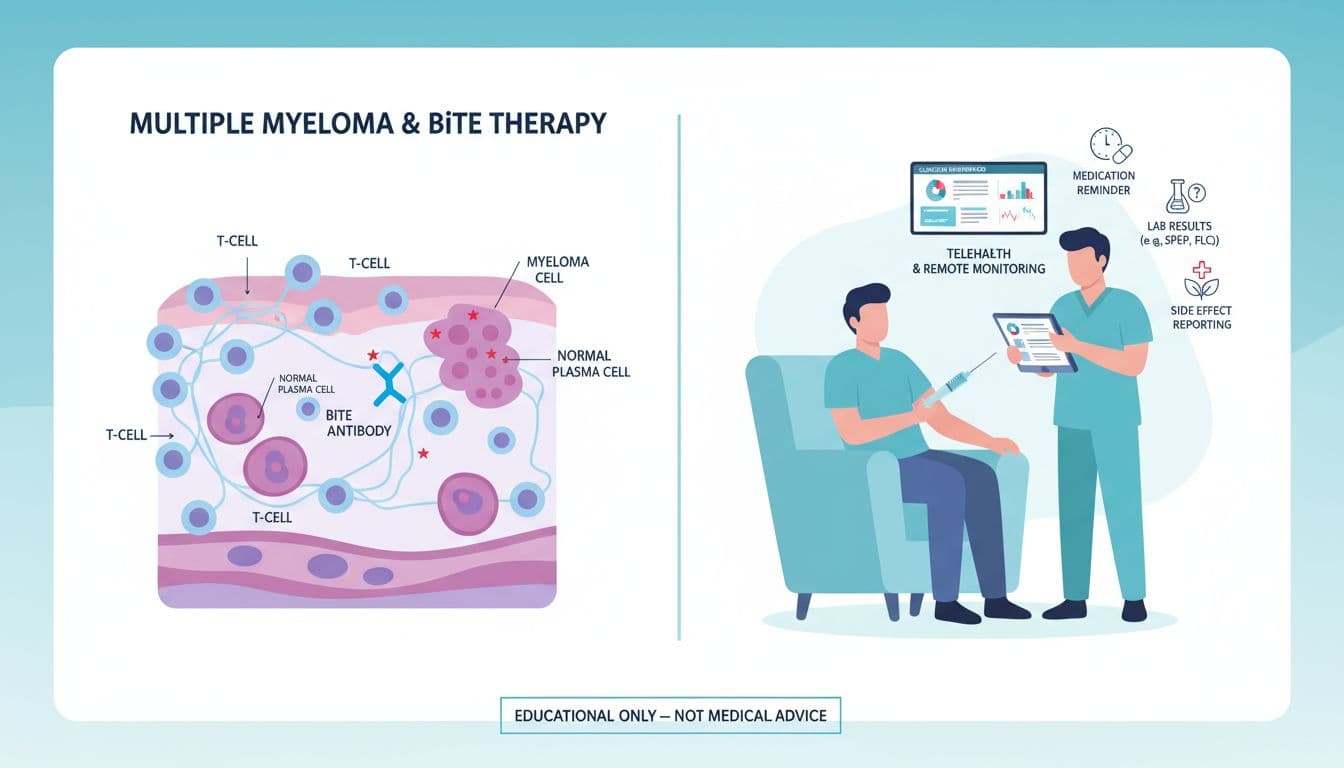
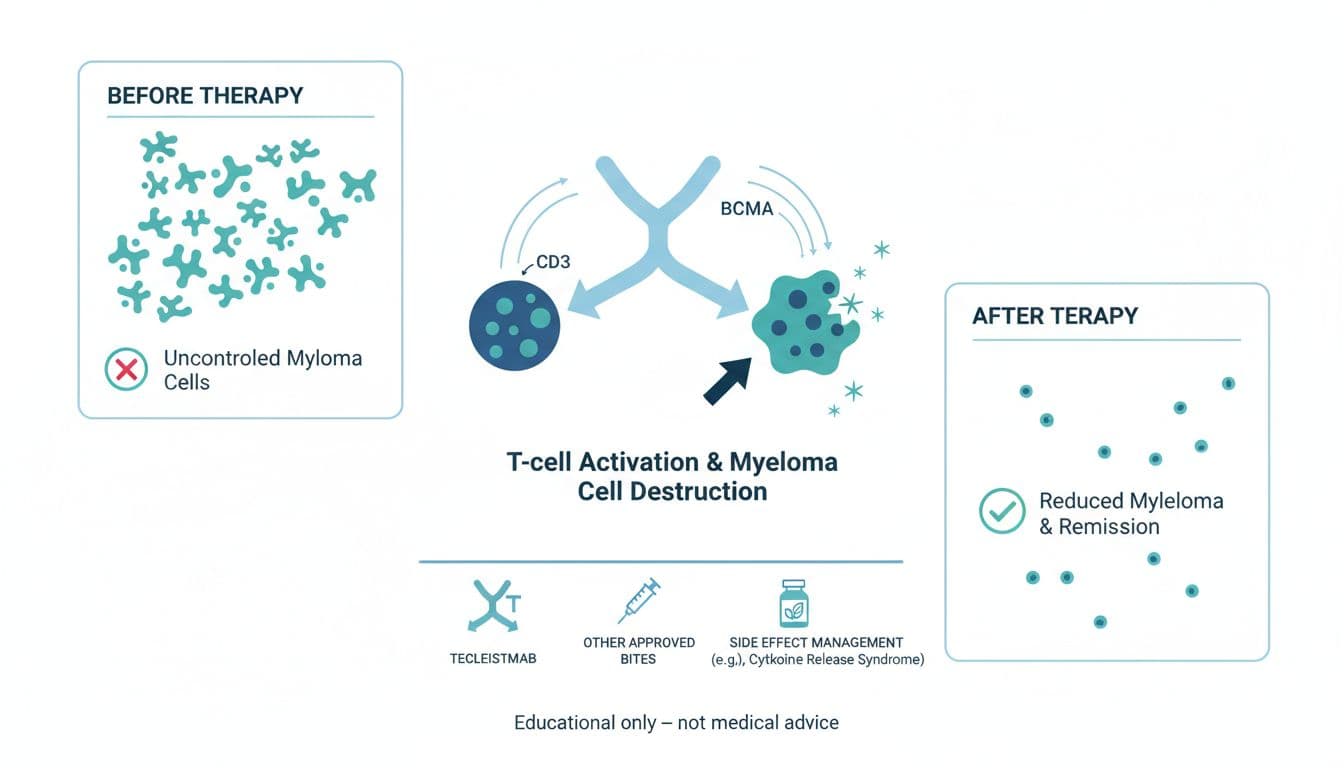
A BiTE is a lab-made antibody with two “hands”:
- One hand holds onto a T cell (an immune cell that can kill abnormal cells).
- The other hand holds onto a marker on a myeloma cell (often BCMA, sometimes GPRC5D).
When those two hands lock in, the BiTE brings the T cell close enough to attack the myeloma cell. Think of it like a tiny matchmaker that forces an introduction your immune system might otherwise miss.
For a helpful big-picture overview of treatments that may show up across the course of myeloma, including bispecific antibodies, Medscape keeps an updated clinical summary on multiple myeloma treatment and management.
How BiTE therapy works (without the heavy science)
Here’s the simplest way to picture it: a myeloma cell is hiding in plain sight, and a T cell is nearby but not reacting. The BiTE connects them, and that connection flips the “go” switch for the T cell.
This matters because myeloma can be skilled at evading immune attention. BiTEs are one way doctors try to narrow that gap.
Where BiTE therapy fits in multiple myeloma therapy (as of late 2025)
BiTE therapy has moved fast in myeloma care. As of late 2025, several bispecific antibodies are in routine use for relapsed or refractory multiple myeloma (when the disease returns or stops responding to other treatments). Common examples include BCMA-targeting drugs (such as teclistamab and elranatamab) and a GPRC5D-targeting drug (talquetamab).
If you want a patient-friendly explanation of why additional BiTE approvals mattered, the AACR Foundation has a clear update on a second BiTE approved for multiple myeloma.
Real-world research is also helping doctors understand what happens outside of tightly controlled trials. For example, the International Myeloma Working Group reported outcomes in broader patient groups in this real-world evaluation of teclistamab.
How it’s given, and why the start can feel intense
BiTE therapy is often started with “step-up” doses. The first days can involve closer monitoring, sometimes in the hospital, because the immune system can react strongly at the beginning. After that, many patients receive doses as outpatient injections on a set schedule.
That early stretch can feel like holding your breath. It helps to name it for what it is: a carefully watched ramp-up, not a personal failure if you need extra support.
The “bytes” that matter: tech support that can make treatment feel less chaotic
Even when “Byte Therapy” really means BiTE, the word “byte” still fits in one practical way: small pieces of tech can hold the boring, repeatable work your brain shouldn’t have to carry.
Used well, technology doesn’t replace your care team. It supports you between visits.
Examples that often help during BiTE therapy:
- Medication reminder alarms (especially on days when fatigue is loud)
- A simple symptom log (fever, chills, cough, sore throat, mouth changes, taste changes)
- A notes app for questions that pop up at 2 a.m.
- Telehealth check-ins when travel is hard
- Patient portals that track labs over time (so trends feel less mysterious)
One gentle warning: don’t let apps turn you into a full-time investigator of your own body. Data should serve you, not haunt you. If tracking starts feeding anxiety, it’s okay to scale back.
Side effects, safety, and the courage of speaking up early
BiTE therapy can work well, but it can also bring real risks. Common concerns include fever and immune reactions early on, low blood counts, and infections. Some people also deal with skin, mouth, or taste changes, depending on the target of the drug.
Here’s what courage looks like in this part: reporting symptoms early, even if you worry you’re “overreacting.” You’re not. Your care team would rather hear from you on day one than on day five.
If your clinic gives you a threshold like “call for fever over 100.4°F (38°C),” treat that like a guardrail, not a suggestion. And ask about prevention steps that may apply to you, such as vaccines, immune globulin, or anti-infection medicines.
For a plain-language look at what’s changing in treatment options and how experts think about newer therapies, Cleveland Clinic shares an accessible overview of what’s new and on the horizon for treating multiple myeloma.
Questions to ask your team if BiTE therapy is on the table
You don’t need perfect words. Bring the messy ones. Still, these questions can help you feel steadier:
- What goal are we aiming for right now, symptom relief, deep response, or remission?
- Why are you recommending this BiTE now, and what are the other options?
- What does the first week look like, and will I need hospital monitoring?
- What side effects should trigger an urgent call, day or night?
- How will we prevent infections, and what symptoms matter most?
- What does success look like on my labs, and how often will we check?
Write the answers down, or record them if the clinic allows it. Memory gets slippery under stress.
Conclusion: Courage is built in small “yes” moments
Treatments change. Your numbers may rise, then fall, then rise again. Through it all, courage doesn’t always roar. Sometimes it’s just the next small “yes,” yes to the appointment, yes to the walk around the block, yes to asking for help.
If “Byte Therapy” means BiTE therapy for you, let the facts ground you, and let hope stay practical. The goal is not to be fearless. The goal is to keep choosing care, one day at a time, and to keep making room for the possibility of remission.

